Ulcerative colitis;
I've said it before and I'll say it again microbiome, microbiome, microbiome
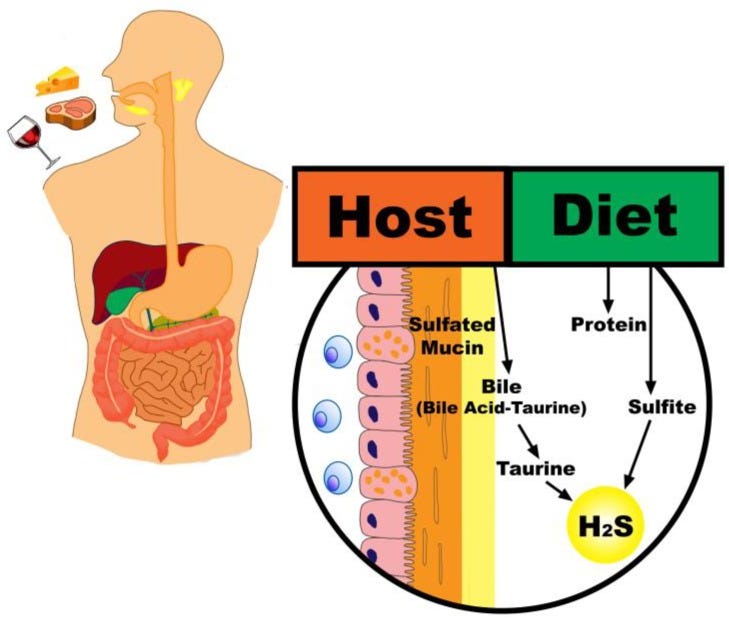
The major risk factors for Ulcerative Colitis, characterised by bloody stools, diarrhoea, hydrogen sulphide production and inflammation in the colon are; diets high in meat, high in sulphur containing amino acids cysteine and methionine (found mostly in animal products), diets low in fibre and alcohol consumption.
Diet and risk of inflammatory bowel disease A diet high in protein, particular animal protein, may be associated with increased risk of inflammatory bowel disease and relapses. N-6 polyunsaturated fatty acids may predispose to ulcerative colitis whilst n-3 polyunsaturated fatty acid may protect. These results should be confirmed in other countries and in younger subjects before dietary counselling is recommended in high risk subjects.
Influence of dietary factors on the clinical course of ulcerative colitis: a prospective cohort study Potentially modifiable dietary factors, such as a high meat or alcoholic beverage intake, have been identified that are associated with an increased likelihood of relapse for UC patients.
A high intake of dairy products or low dietary fibre intake may be associated with relapse10–14 but the strongest evidence for a dietary factor is that sulphur and sulphate may be implicated in relapse of colitis.
A high meat, protein, or alcohol intake is associated with an increased risk of relapse which may well occur because these foods are rich sources of sulphur and sulphate which increase the concentration of faecal hydrogen sulphide that is toxic to the colonocyte.
Dietary Factors in Sulfur Metabolism and Pathogenesis of Ulcerative Colitis A compelling case does exist that a typical western diet, which tends to be high in protein and low in fermentable fiber, may promote the accumulation of harmful products such as H2S and even increase their toxicity, and is also associated with a lower production of beneficial products such as butyrate
The high protein content of animal-based diets provides a greater amount of sulfur that becomes available to distal gut microbiota [19]. Additionally, the higher fat content of a typical animal-based diet may lead to an increase in taurine conjugation to bile acids and a corresponding increase in the quantity of sulfur in the colonic lumen through an endogenous source [20]. Importantly, an animal-based diet pattern will also tend to be low in fiber, which may drive a metabolic shift of microbiota away from carbohydrate and towards protein fermentation and increased mucin degradation
Onset of Ulcerative Colitis during a Low-Carbohydrate Weight-Loss Diet and Treatment with a Plant-Based Diet: A Case Report A man, 172 cm in height and weighing 72 kg, at age 36 years followed a low-carbohydrate weight-loss diet. His weight decreased to 66 kg as desired. Thereafter he noticed bloody stool. Colonoscopy revealed diffuse inflammation limited to the rectum, and he was diagnosed with ulcerative colitis. He underwent an educational hospitalization for ulcerative colitis. A plant-based/semivegetarian diet was provided during hospitalization. Bloody stool disappeared during hospitalization and he achieved remission without medication for inflammatory bowel disease.
This case indicates that an onset of ulcerative colitis can be an adverse event to a low-carbohydrate weight-loss diet.
Diet-associated gut dysbiosis is becoming a leading environmental factor in a variety of current chronic diseases. A plant-based diet is advocated to counter these diseases. Ulcerative colitis is not an exception. A novel frontline approach consisting of dietary manipulation (ie, semivegetarian diet) induced remission without medication in this case.
Relapse Prevention in Ulcerative Colitis by Plant-Based Diet Through Educational Hospitalization: A Single-Group Trial To date, adherence to 5-aminosalicylic acid in the quiescent stage has been advocated to prevent a relapse.13–15,18 Kawakami et al15 used the same definition of relapse that we did in a study of Japanese patients who were in remission for more than 6 months, and they reported a relapse rate at 1 year of 41% for nonmedication-adherent patients and 16% for medication-adherent patients. Reports of this kind have been the basis for lifelong maintenance medication in UC.13–15
Our relapse rate of 2% at 1 year is far better than that previously reported.
We believe that IBD is a lifestyle disease mediated mainly by a westernized diet. It is suggested that patients can stop medication when they feel confident after a few years of remission using the PBD
Relapse Prevention by Plant-Based Diet Incorporated into Induction Therapy for Ulcerative Colitis: A Single-Group Trial The relapse rate for initial episode cases of UC after treatment incorporating PBD on an inpatient basis during the induction phase was 14% at 1 year (a relapse rate of 28% to 68% in other studies using drug therapy, which have side effects such as diarrhoea and stroke) and 27% at 5 years (58% to 75% relapse in studies using drug therapy), which were far lower than those reported with conventional treatment. Significantly higher PBDS was observed compared with baseline even after 6 years of follow-up. A PBD was found to be effective in prevention of UC relapse
A diet high in animal products has a clear pathogenesis for UC; sulphur containing amino acids found mostly in meat and the overgrowth of bile loving bacteria from consuming saturated animal fats both produce hydrogen sulphide.
Beneficial bacteria which protect colonocytes thrive on fibre and insoluble starches found only in whole food plant based diets.
Jo
🐒




I appreciate the helpful info as someone close to me is living with this condition.
I used to experience very uncomfortable bloating and acid reflux after some meals... worked with a dietician on this and determined that garlic and onion (particularly raw) were the culprits...
I eliminated both and the problems ended.
From time to time I will have pizza made by an Italian outfit that is just too good to resist... the sauce is loaded with garlic and I pay the price afterwards -- but it's worth it!
I know quite a few people who go through their entire lives not working out that diet is causing the problem... a friend of mine died at 40 from esophageal cancer ---I recall him complaining that he had really bad acid reflux for years ... and that is a leading cause of this type of cancer.
If we consider the impact of caffeine and sugar on the body - why wouldn't other types of foods also have dramatic impacts as well.
I suspect a wide range of illnesses could be eliminated by changes in diet -- there are the obvious ones like eliminating junk food ... but more subtle ones like cutting out garlic and onion.
Check this out https://www.hopkinsmedicine.org/health/wellness-and-prevention/fodmap-diet-what-you-need-to-know